Obsessive Compulsive Disorder
Obsessive-Compulsive Disorder (OCD) is a common yet misunderstood mental health condition marked by distressing obsessions and time-consuming compulsions. This blog from Ms. Keerthana Vummadisingu, offers in-depth insights into OCD symptoms, causes, and evidence-based treatments like CBT and ERP.
Keerthana Vummadisingu, MSc, Mphil - Clinical Psychology


Obsessive Compulsive Disorder (OCD) is a mental health condition in which people have obsessions which are recurrent and persistent urges, thoughts or images that are experienced as intrusive and unwanted and cause significant distress or anxiety. To alleviate this distress, individuals engage in compulsions which are repetitive behaviors or mental acts they feel driven to perform. These compulsions are intended to reduce the anxiety associated with the obsessions or to prevent a feared event or situation, even if the actions are not logically connected to the feared outcomes. The obsessions and compulsions are time consuming and significantly disrupt the person’s daily routine, occupational functioning, social activities, and interpersonal relationships. An individual with OCD can have obsessions, compulsions, or both.
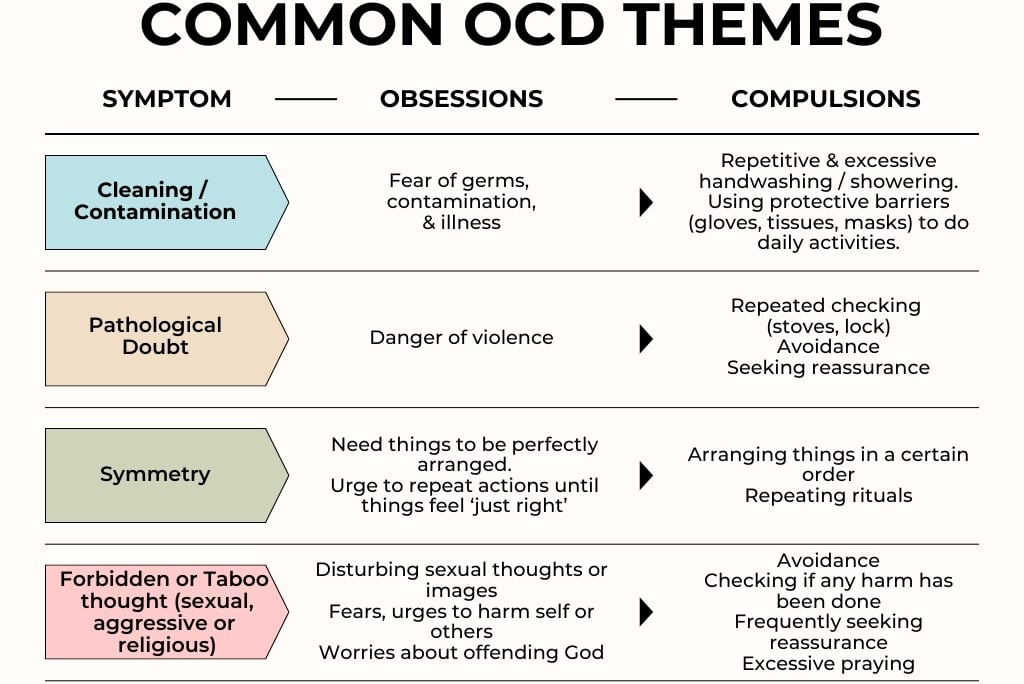
Commonly seen themes in OCD
OCD is the most fourth most common psychiatric diagnosis. The mean age of onset is about 20 years although men can have a slightly earlier age of onset compared to women. The onset of the disorder can occur in adolescence or childhood and sometimes as early as 2 years of age. The types of obsessions and compulsions one has can also vary over time.
What causes OCD?
While the exact cause is unknown, multiple contributing factors shape OCD
Biological factors
Imbalances in serotonin and dopamine systems play distinct roles: reduced serotonin activity is associated with recurrent intrusive thoughts (obsessions), while abnormal dopamine signaling contributes to the ritualistic, repetitive behaviors observed in the disorder.
Genetic studies show heritability at 40–50%, with specific genes (e.g., SLC1A1) implicated.
Psychological factors
Cognitive distortions: Individuals with OCD often exhibit dysfunctional beliefs, including perfectionism, intolerance of uncertainty, and an inflated sense of responsibility. These cognitive distortions can lead to misinterpretation of intrusive thoughts as significant or threatening, prompting compulsive behaviors to alleviate distress.
Behavioral conditioning: People with OCD associate certain objects or situations with fear, avoiding those things by performing "rituals." These rituals temporarily reduce distress, making repetitions more likely.
Environmental influences
Several environmental factors have been linked to an increased risk of developing OCD. These include complications around the time of birth, such as premature delivery and adverse perinatal events, as well as prenatal exposures like maternal smoking.
Childhood experiences of physical or sexual abuse, along with other stressful or traumatic events, can also contribute.
In some cases, children may experience a sudden onset of obsessive-compulsive symptoms, which has been associated with environmental triggers such as certain infections or post-infectious autoimmune responses.
When should one seek professional help for OCD?
Not all repetitive thoughts or behaviors indicate OCD.
Everyone may occasionally double-check or overthink things, but in OCD, these experiences become much more intense and disruptive. People with OCD typically:
Struggle to control their obsessions or compulsions, even when they recognize them as irrational or excessive.
Spend a significant amount of time, often more than an hour daily engaging in these thoughts or behaviors.
Do not experience enjoyment from the compulsions but may feel brief relief from anxiety.
Avoidance of certain people, places or activities to prevent triggers of obsessions or compulsions becomes common.
Face serious disruptions in their daily life, work, or relationships due to these symptoms.
How is OCD treated?
In most cases treatment for OCD involves a combination of psychotherapy and medication.
Psychotherapy is an effective treatment for both adults and children with OCD. Studies show that evidence-based therapies, especially cognitive-behavioral approaches like Exposure and Response Prevention (ERP), can be just as effective as medication in treating many individuals.
What to expect in psychotherapy?
When a client begins therapy for OCD, the therapist conducts a comprehensive evaluation, often including clinical interviews and standardized tools like the Yale Brown Obsessive Compulsive Scale (Y-BOCS), to identify the specific obsessions and compulsions. Based on this assessment, a tailored treatment plan (such as CBT with ERP, ACT, or another appropriate modality) is developed and initiated.
Cognitive Behavioral Therapy (CBT)
People with OCD possess strong faulty beliefs that arise from cognitive errors. Some of the most seen cognitive errors in OCD are overestimating risk, harm, and danger, overcontrol and perfectionism, persistent doubting, magical thinking. CBT focuses on directly challenging these cognitive errors and the resulting faulty beliefs, a technique called cognitive restructuring.
Exposure and Response Prevention (ERP).
ERP focuses on teaching people to face their fears (the obsessions) and then not do the typical ritual (the compulsion), so their anxiety decreases over time.
Example: Fear of Germs and Hand-WashingIdentify the Fear (Obsession) - Someone feels intense anxiety when they think their hands are dirty even after washing.
Create a Fear Ladder or Hierarchy - The therapist and the person list situations from least to most scary:
Touching a "clean" surface (e.g., their desk).
Touching a door handle in a public bathroom.
Shaking hands with someone they've just met.
Gradual Exposure
They start with the least scary task in the hierarchy.
The person touches the desk but does not wash their hands afterward.
Prevent the Compulsion
They resist the urge to wash till the anxiety drops.
Anxiety might spike but eventually drops on its own.
Repeat and Progress
As anxiety lessens, they move to harder tasks on the heirarchy.
Over time, they learn they can tolerate discomfort and no disaster happens.
Why this works?
Exposure lets them experience fear without escaping it.
Response prevention breaks the habit of ritually "fixing" the fear.
Their brain learns: "My anxiety decreases on its own; washing isn't necessary."
Acceptance & Commitment Therapy (ACT)
ACT helps the clients observe their obsessive thoughts as just mental events without giving them undue power. The therapist guides one to live a value driven, meaningful life even while OCD symptoms are present.
ACT also encourages individuals to accept their intrusive thoughts and urges without judgement rather than fight or suppress them. It helps with cognitive defusion; learning to observe thoughts as sperate from reality and experiencing them without getting entangled. It also encourages individuals to take actions that align with their values, even when it means facing difficult thoughts or feelings.
In addition to these therapies, mindfulness and relaxation strategies are also incorporated to support those with OCD.
In Conclusion
OCD is a complex but treatable condition. Understanding its underlying mechanisms; biological, psychological, and environmental empowers people to seek and receive effective care. From evidence-based ERP therapy to personalized medication plans and mindfulness techniques, many paths can lead to symptom relief. If obsessive thoughts or compulsive behaviors interfere with your life, reaching out to a mental health professional is a brave and essential first step.
Consultant Clinical Psychologist
Asha Neuromodulation Clinics (ANC) - Kokapet
MSc, Mphil - Clinical Psychology
References:
American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.)
Sadock, B. J., Sadock, V. A., & Ruiz, P. (2015). Kaplan & Sadock’s synopsis of psychiatry: Behavioral sciences/clinical psychiatry (11th ed.). Philadelphia, PA: Wolters Kluwer.
Barlow, D. H., Durand, V. M., & Hofmann, S. G. (2018). Abnormal psychology: An integrative approach (6th ed.). Belmont, CA: Wadsworth Cengage Learning
Mayo Clinic Staff. (2023, June 23). Obsessive-compulsive disorder (OCD): Symptoms & causes. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/obsessive-compulsive-disorder/symptoms-causes/syc-20354432
National Institute of Mental Health. (n.d.). Obsessive-compulsive disorder (OCD) [Statistics]. U.S. Department of Health and Human Services. Retrieved June 13, 2025, from https://www.nimh.nih.gov/health/statistics/obsessive-compulsive-disorder-ocd
Mercy. (n.d.). Obsessive compulsive disorder. Mercy. Retrieved June 13, 2025, from https://www.mercy.net/service/obsessive-compulsive-disorder
National Institute of Mental Health. (2023, September). Obsessive-compulsive disorder: When unwanted thoughts or repetitive behaviors take over (NIH Publication No. 23-MH-4676) [Brochure]. U.S. Department of Health and Human Services.
Cleveland Clinic. (n.d.). Obsessive-compulsive disorder (OCD): Symptoms & treatment [Health Encyclopedia]. Retrieved June 13, 2025, from https://my.clevelandclinic.org/health/diseases/9490-ocd-obsessive-compulsive-disorder#diagnosis-and-test
Asha Neuromodulation Clinics (ANC) - Kokapet
A Premier Psychiatric Clinic-cum-Neuromodulation Center
For Appointments
E-mail: contact@anc-kokapet.com
Call: +91 707 5565 262
© 2025. All rights reserved.
clinic timings
Monday to Saturday - 10 am to 8 pm
** Sunday Closed **


Scan for location